The shift to a value-based reimbursement model may cause alterations in revenue cycle management. Value-based reimbursement replaces the fee-for-service structure, and healthcare professionals should be prepared to adapt to the changes being made. The shift influences efficient revenue cycle management and presents revenue cycle management consulting opportunities.
Here are a few ways value-based reimbursement impacts revenue cycle management:
What is Revenue Cycle Management?
Revenue Cycle Management (RCM) is the financial heartbeat of healthcare, orchestrating the entire journey from patient appointment to payment. It’s a strategic process vital for healthcare organizations, ensuring smooth financial operations.
Think of it as the conductor guiding billing, coding, claims, and payments to create a harmonious financial symphony. By optimizing RCM, providers can enhance efficiency, minimize errors, and improve overall financial health.
As highlighted by industry experts (insert reference). RCM is not just about numbers; it’s a dynamic crucial for sustaining healthcare organizations and providing quality patient care.
Why is Revenue Cycle Management Important in Healthcare?
Revenue Cycle Management (RCM) is the financial backbone of healthcare, ensuring the smooth flow of financial transactions from patient service to reimbursement. This strategic process not only optimizes billing and payment collection but also enhances the overall financial health of healthcare organizations.
By minimizing errors and streamlining billing processes, RCM allows healthcare providers to focus on delivering quality patient care without compromising financial stability.
As noted in industry insights (insert relevant references), effective. Revenue Cycle Management is paramount for healthcare providers navigating the complexities of reimbursement, coding, and evolving healthcare policies.
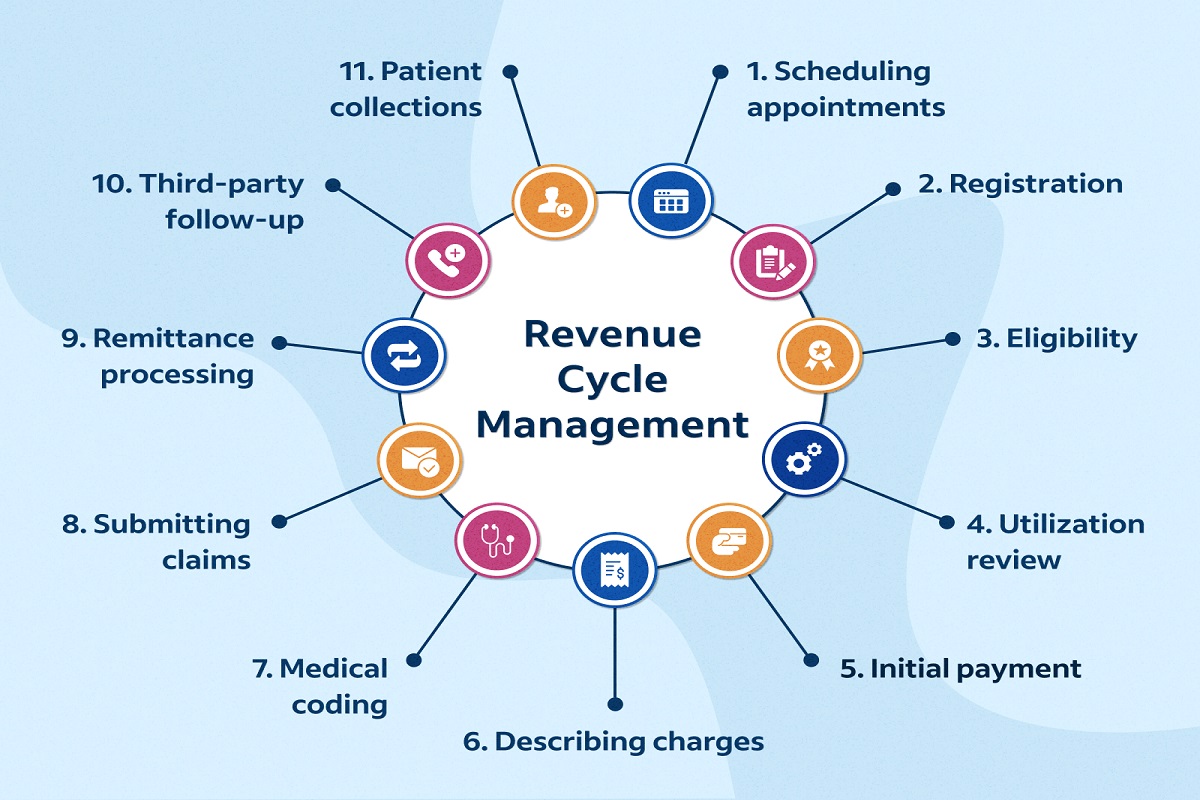
What Steps Does Revenue Cycle Management Encompass?
Revenue Cycle Management (RCM) is a comprehensive process within healthcare that involves a series of strategic steps to ensure the financial health of healthcare organizations.
Here’s an overview of the key steps encompassed by RCM:
- Patient Registration: The RCM journey begins with accurate and detailed patient registration, capturing essential demographic and insurance information.
- Insurance Verification: RCM involves validating patient insurance coverage to avoid billing discrepancies and streamline claims processing.
- Coding: Accurate medical coding is crucial for proper reimbursement. RCM includes meticulous coding of medical procedures and diagnoses.
- Charge Capture: Capturing charges for services rendered ensures that all billable activities are accounted for in the billing process.
- Billing: RCM incorporates the creation and submission of accurate and timely bills to insurance providers or patients, reflecting the services provided.
- Claims Submission: Efficient RCM includes the timely submission of claims to insurance companies, reducing the likelihood of denials and delays in reimbursement.
- Payment Posting: Once payments are received, RCM involves posting and reconciling payments to ensure accurate financial records.
- Denial Management: Addressing and resolving claim denials is a vital aspect of RCM to optimize revenue and reduce financial setbacks.
- Patient Collections: RCM extends to managing patient collections. Ensuring clear communication about financial responsibilities and facilitating payment.
Understanding these key steps and their seamless integration is fundamental for healthcare organizations aiming to optimize their revenue cycles.
Reference: Healthcare Revenue Cycle Management Market – Growth, Trends, COVID-19 Impact, and Forecasts (2021 – 2026).
Value-Based Reimbursement
The payment model rewards healthcare providers based on the quality of care evidenced by patient outcomes. Healthcare providers receive payments according to quality factors like patient satisfaction rates, readmissions, and general health outcomes.
The reimbursement that is based on quality encourages providers to focus on lowering hospital readmissions, preventive care, and enhancing overall patient health.
Focusing on patient health outcomes helps lower healthcare costs by decreasing the need for continuous care and reducing spending.
Adopting Value-Based Reimbursement
Healthcare providers can invest in professional revenue cycle management consulting and technologies such as electronic health records (EHRs) to equip value-based reimbursement. The technologies enable tracking and reporting performance to determine patients’ outcomes that need improvement.
Providers can increase coordination with other professionals, healthcare providers, and patients to enhance patient outcomes and increase revenue.
Healthcare providers may also increase the adoption of evidence-based practices to meet the quality measures necessary for better patient outcomes and increased revenue.
Impact on Revenue Cycle Management
The value-based reimbursement approach requires a shift in the focus of revenue cycle management to patient outcomes. Healthcare providers focusing on offering services can now prioritize collaboration and coordination to improve patient outcomes. This enables the prevention of redundant processes that may increase overhead costs.
The value-based reimbursement approach helps healthcare providers lower denied claims by backing claims with patient outcomes. This reimbursement method also influences the incorporation of data-driven decisions to pinpoint areas requiring improvement, optimize patient outcomes, and increase revenue.
Benefits of Value-Based Reimbursement
The value-based reimbursement model influences focus on preventive care and improved coordination, helping healthcare providers have better outcomes. Preventive care can lead to lower health costs and increased patient satisfaction.
They impact a lesser demand for expensive medical processes and decreased patient stays. Value-based reimbursement may lower the administrative burden of patient care. This is done by improving coordination between healthcare professionals and other experts and increasing data accuracy. Data accuracy may reduce costly errors and make sure healthcare practitioners are reimbursed on time.
The reimbursement model increases the likelihood of cost savings and better financial performance by lowering patient readmissions and redundant processes. Lower administration costs resulting from coordination between professionals enhance financial performance by improving cash flow.
Value-based reimbursement improves the quality of financial decisions by depending on data analysis of patient outcomes to identify areas needing improvement.
Challenges of Value-Based Reimbursement
Some healthcare providers may resist the shift to a value-based reimbursement model. It is might be difficult for healthcare professionals to invest in the necessary infrastructure and resources to support value-based reimbursement. The complex rules of value-based reimbursement may pose a challenge to healthcare providers required to follow defined reporting rules, payment models, and measures of quality.
Small healthcare facilities may be unable to purchase integrated technologies necessary for a value-based reimbursement .
Consider Revenue Cycle Management Consulting for Value-Based Reimbursement Today
The healthcare sector’s shift to a value-based model prompts healthcare providers to adapt to the challenge of the new payment format. Investments in stronger coordination with other professionals, technology, and infrastructure and prioritizing patient outcomes can enable healthcare providers to adapt to the value-based model and experience its benefits.
The payment model enhances healthcare quality by reimbursing based on patient outcomes, and its application can lead to quality care and better patient outcomes.
Frequently Asked Questions about Revenue Cycle Management (RCM):
A1: Revenue Cycle Management (RCM) is a strategic process in healthcare. It involves the financial management of patient services. From appointment scheduling and billing to payment collection.
A2: RCM ensures the financial health of healthcare organizations by optimizing the entire patient care financial process. It streamlines billing, reduces errors, and enhances revenue capture.
A3: RCM includes patient registration, insurance verification, coding, charge capture, billing, claims submission, payment posting, denial management, and patient collections. It covers the entire financial life cycle of a patient’s interaction with a healthcare provider.
A4: Efficient RCM positively affects patient care by minimizing administrative burdens, reducing billing errors, and accelerating the reimbursement process. This allows healthcare providers to focus more on delivering quality patient care.
A5: Yes, effective RCM can significantly enhance financial performance by accelerating cash flow, reducing billing delays, and minimizing claim denials. It helps healthcare organizations optimize revenue streams.
A6: Yes, RCM is influenced by evolving healthcare policies, reimbursement models, and coding regulations. Staying updated on industry changes is crucial to adapting RCM strategies accordingly.
A7: Implementing RCM s involves selecting appropriate software, staff training, and ongoing monitoring. Collaborating with RCM experts or outsourcing services can also optimize implementation.
A8: Metrics include days in accounts receivable (AR), clean claims rate, denial rate, and patient collection rate. Monitoring and analyzing these metrics help healthcare providers gauge the efficiency of their RCM processes.